Diabetes is a disorder characterized by high blood sugar levels and HbA1c > 6.5. It is commonly differentiated into 2 types – Type 1 and Type 2. Type 1 diabetes is defined by the decreased production of insulin and Type 2 Diabetes is defined by insulin resistance and decreased insulin production. Both Type 1 and Type 2 diabetes have an effect on the bone health and affects the bone mineral density, bone turnover, bone strength and bone structure.
The increased blood sugar levels inhibit and prevent the bone-forming cells (osteoblasts) from building strong bones. The complications of diabetes such as diabetic nephropathy may result in loss of calcium that is required for strong bones. Also certain oral anti-diabetic medications cause bone loss as a side effect.
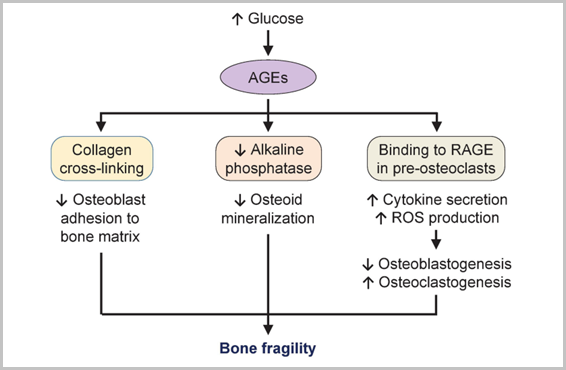
Type 1 diabetes affects bone metabolism by causing accumulations of harmful advanced glycation end products (AGEs). These products prevents the differentiation of osteoblasts, adipocytes, and cartilage and inhibits the osteoblastic synthesis of the protein osteocalcin, resulting in poor bone formation. Also, T1DM affects the microarchitecture of bone by decreasing bone mineral density (BMD).
On the contrary, Type 2 diabetes causes increased BMD and higher the BMD, lower is the overall bone turnover and there is a decreased expression of bone turnover markers. Hyperinsulinemia in patients with T2DM could also be responsible for the increased BMD, as insulin interacts with the IGF-1 receptor present on osteoblasts on account of its structural homology and it is likely that hyperinsulinemia could create the effects similar to IGF-1 by promoting osteoblast division and differentiation.
While type 1 diabetics exhibit low bone mineral density and a six - to sevenfold higher risk for fractures, type 2 diabetes patients exhibit normal to high bone mineral density and up to threefold higher risk for fractures.
Osteoporosis is a condition where the bones of the body become weak and brittle and even mild stress may lead to fracture. Osteoporosis-related fractures mostly occur in the hip, wrist or spine. Diabetic patients, particularly with type 1 diabetes, have poorer bone quality and an increased risk for fractures. Diabetes mellitus (DM) increases the function of osteoclast (bone resorption) and decreases the osteoblast (bone-forming) function, leading to accelerated bone loss, osteopenia and osteoporosis.
Insulin has an anabolic effect on bone and stimulates the osteoblast differentiation, enhancing the production of osteocalcin, thus helping in bone formation. The Thiazolidinediones (Pioglitazone – Pioz 15mg, Pionorm 15mg), a class of antidiabetic drugs, are categorized as drugs causing secondary osteoporosis, owing to their effect in bone loss and further increase of facture risk, especially in older women. On the contrary, metformin and sulfonylureas does not have a negative effect on bone health and may, in fact, protect against fragility fractures.
 Medinexus, an app dealing with childhood obesity launched
Medinexus, an app dealing with childhood obesity launched
 Conference on Diabetes
Conference on Diabetes
 Navigating Hyperthyroidism from diagnosis to care
Navigating Hyperthyroidism from diagnosis to care
Copyright @2022 Dr Suresh Damodharan. Designed and Maintained by ITindustries.com